September 7, 2024
6 Ways To Treat Bladder Leak
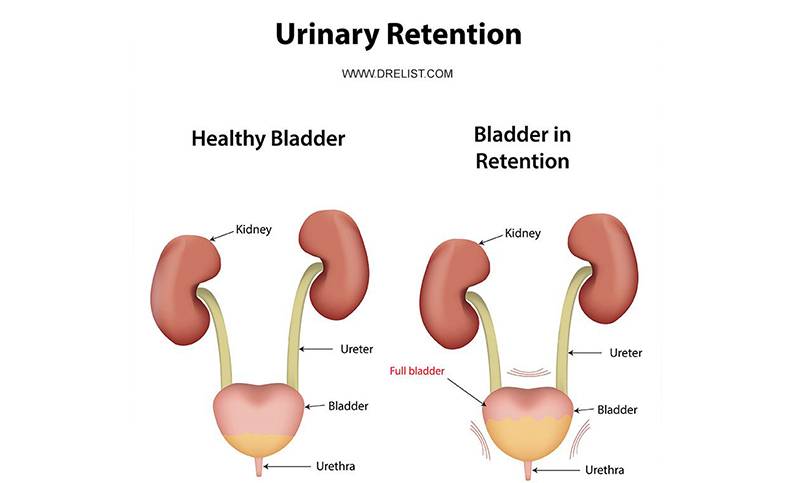
Management Of Urinary Incontinence In Postmenopausal Females: An Emas Medical Overview From adolescence to menopause, hormone changes can affect the strength and feature of the pelvic floor muscular tissues, usually causing urinary concerns such as stress urinary incontinence (SUI). A big component of this is due to pregnancy, giving birth and menopause. Each of these occasions in a female's life can lead to bladder control problems. Pregnancy can be a temporary reason for incontinence and the bladder control problems normally improve after the child is birthed. Some women experience urinary incontinence after delivery as a result of the stress giving birth handles the pelvic floor muscles. When these muscular tissues are deteriorated, you're more likely to experience leakage problems. Mild electric stimulation can be effective for tension urinary incontinence and urge urinary incontinence, yet you may require multiple treatments over numerous months. Obstructive problems must be handled as swiftly as feasible. Urinary system system infection must be treated with ideal medical treatment. Ectopic ureters and various other hereditary anomalies can be surgically corrected; the clinician should understand that functional problems of urinary system bladder storage space or urethral capability may accompany this problem.Urinary Conditions
These hormonal shifts can affect bladder function and urinary system habits, showing up as urinary symptoms such as boosted frequency, necessity, or leakage. Reduced levels of estrogen and urinary system incontinence go hand in hand. As females age and begin coming close to menopause, the ovaries reduce the process Helpful site of making estrogen, and the levels of this women sex hormone normally decrease in the body. [newline] Ultimately, with menopause, the production of estrogen quits, and this influences the body in many ways. Without estrogen, women find it challenging to keep healthy urologic features throughout and after menopause. Bladder control for women starts together with their final menstrual duration and raises afterwards.Exactly How Is Incontinence Treated?
These medicines all have the possible to trigger restlessness, tachycardia and high blood pressure. Ephedrine is provided at a dose of 4 mg/kg every 8 to 12 hours. Lots of big type canines might be started on 25 mg every 8 hours, increasing the dosage to 50 mg if there is no clinical reaction at the lower dose. Phenylpropanolamine has the very same potency and pharmacologic homes as ephedrine yet appears to create less central nerves stimulation. The suggested dosage is 1.5 to 2.0 mg/kg twice daily to 3 times daily. Pseudoephedrine resembles ephedrine and phenylpropanolamine.Exactly How Can I Minimize My Danger Of Tension Incontinence?
During this procedure, the posterior wall of the urethra shears off the anterior urethral wall surface to open up the bladder neck when inherent sphincter deficiency exists. Useful urinary incontinence is the inability to hold urine as a result of factors other than neuro-urologic and reduced urinary system dysfunction. Videourodynamic research studies are scheduled to examine complicated cases of stress and anxiety urinary incontinence.- Double-contrast cystography may be indicated for full visualization of the urinary system bladder and recognition of urinary bladder lesions.
- Endocervix glandular cells activity during menopause and consequently the amount of mucin decreases that this creates to vaginal dryness that develops as a primary issue in postmenopausal females.
- In psychophysiological feedback, a cord is attached to an electric patch over your bladder and urethral muscular tissues.
- Prompt urinary incontinence is much more widespread after the menopause, and the peak occurrence of stress urinary incontinence occurs around the time of the menopause.
- These hormonal shifts can influence bladder function and urinary system routines, showing up as urinary symptoms such as enhanced regularity, urgency, or leak.
- Anxiety urinary incontinence develops when task places enhanced stress on your bladder.
Why do I leak urine after my period?
- Hormonal agents impact hair's all-natural cycle and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and sleep issues.Digestive distress. Hormonal agent control or birth control medication.Hormone replacement medications.Anti-androgen medications.Vaginal estrogen.Clomiphene and letrozole.Assisted reproductive
- technology.Metformin.Levothyroxine. Antidiuretic hormone('ADH)is a chemical created in the brain that triggers the kidneys to release much less water, reducing the quantity of urine created. A high ADH level triggers the body to generate much less pee.
Social Links