September 10, 2024
The Effects Of Hormones On Urinary System Incontinence In Postmenopausal Women

The Duty Of Hormones In Female Urinary System Health If left neglected, these skin disorders may result in pressure sores and abscess, potentially causing secondary infections. The exact occurrence of urinary incontinence is hard to approximate. Component of the difficulty has actually been in specifying the degree, amount, and frequency of urine loss essential to qualify as pathologic, with varying meanings among studies.
What Are The Problems Of Tension Incontinence?
Just how to treat hormonal agent imbalances?
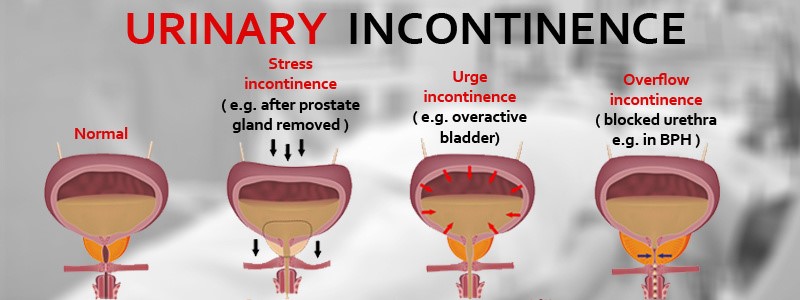
Somatic and free nerves carry bladder volume input to the spinal cord, and motor output innervating the detrusor, sphincter, and bladder musculature is adjusted appropriately. The cortex exerts a predominantly inhibitory influence, whereas the brainstem facilitates peeing by working with urethral sphincter relaxation and detrusor contraction. Just 5% of individuals who are incontinent and 2% of assisted living home homeowners that are incontinent obtain proper medical examination and treatment.
Mayo Facility Press
Low estrogen can trigger bladder signs and symptoms by thinning the cells that lines the vagina. This decreases the flexibility and stamina of the vaginal canal and surrounding muscles, lowering muscle mass support for the bladder and relevant structures, such as the urethra. However, not all people with reduced estrogen establish bladder concerns. For instance, individuals who have formerly delivered may have pelvic floor disorder.
- As your uterus stretches to hold the growing baby, a couple of points take place.
- Intrinsic sphincter deficiency, resulting from loss of function of both the interior and the outside sphincter device, is the only cause of tension urinary incontinence in men.
- Diethylstilbestrol is normally carried out at a dosage of 0.1 to 1.0 mg/dog once daily for 5 to 7 days and after that as soon as weekly or much less as needed to preserve continence.
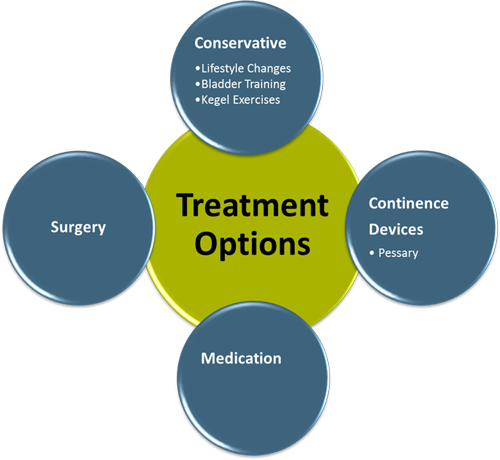
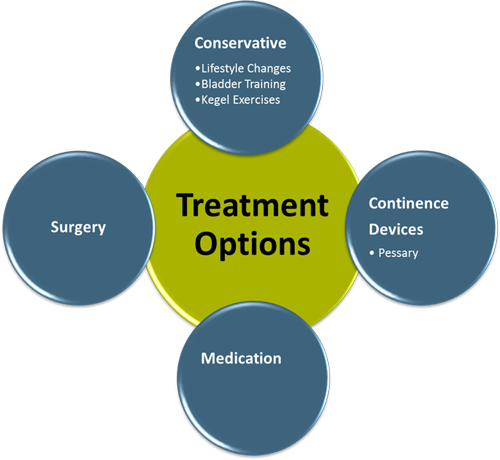
Depending upon the seriousness of the stress and anxiety incontinence, dripping urine may be an inconvenience or embarrassing. Lots of people can enhance their symptoms by consistently doing pelvic flooring exercises. For modest to extreme stress urinary incontinence, tools, injections or surgeries can aid. A much less usual cause is an intrinsic sphincter deficiency, usually additional to pelvic surgeries. In either situation, urethral sphincter function suffers, resulting in urine loss at lower than common abdominal pressures. Estrogen, recognized for its function in maintaining the wellness of urogenital tissues, contributes to the stability and flexibility of
Urinary incontinence the pelvic flooring muscular tissues. Nonetheless, changes in estrogen levels throughout the menstruation can influence bladder muscle mass tone, causing signs like urinary system seriousness and enhanced level of sensitivity to bladder pressure. The function of estrogen and progesterone and p53, in developing prolapse of pelvic organ and stress and anxiety urine incontinence is reported in numerous research study studies [19] That based upon the subject of this post, a number is mentioned. Outcomes of different research studies reveal that vaginal atrophy, uterine prolapse, cystocele, Rectocele, Ectropion, cervix abscess and irritation in women boosts. The urethral disorder, nighttime enuresis, urinary system tract infection is reported in 7% - 10% of postmenopausal ladies [20] In a study by Zhu and his coworkers, the level of estrogen receptor in tissues of Pelvic floor of clients with stress and anxiety incontinence was reported substantially lower than the control group [22]